113 Bacterial Diseases in Humans
Learning Objectives
By the end of this section, you will be able to do the following:
- Identify bacterial diseases that caused historically important plagues and epidemics
- Describe the link between biofilms and foodborne diseases
- Explain how overuse of antibiotics may be creating “super bugs”
- Explain the importance of MRSA with respect to the problems of antibiotic resistance
To a prokaryote, humans may be just another housing opportunity. Unfortunately, the tenancy of some species can have harmful effects and cause disease. Bacteria or other infectious agents that cause harm to their human hosts are called pathogens. Devastating pathogen-borne diseases and plagues, both viral and bacterial in nature, have affected humans and their ancestors for millions of years. The true cause of these diseases was not understood until modern scientific thought developed, and many people thought that diseases were a “spiritual punishment.” Only within the past several centuries have people understood that staying away from afflicted persons, disposing of the corpses and personal belongings of victims of illness, and sanitation practices reduced their own chances of getting sick.
Epidemiologists study how diseases are transmitted and how they affect a population. Often, they must following the course of an epidemic—a disease that occurs in an unusually high number of individuals in a population at the same time. In contrast, a pandemic is a widespread, and usually worldwide, epidemic. An endemic disease is a disease that is always present, usually at low incidence, in a population.
Long History of Bacterial Disease
There are records about infectious diseases as far back as 3000 B.C. A number of significant pandemics caused by bacteria have been documented over several hundred years. Some of the most memorable pandemics led to the decline of cities and entire nations.
In the 21st century, infectious diseases remain among the leading causes of death worldwide, despite advances made in medical research and treatments in recent decades. A disease spreads when the pathogen that causes it is passed from one person to another. For a pathogen to cause disease, it must be able to reproduce in the host’s body and damage the host in some way.
The Plague of Athens
In 430 B.C., the Plague of Athens killed one-quarter of the Athenian troops who were fighting in the great Peloponnesian War and weakened Athens’s dominance and power. The plague impacted people living in overcrowded Athens as well as troops aboard ships that had to return to Athens. The source of the plague may have been identified recently when researchers from the University of Athens were able to use DNA from teeth recovered from a mass grave. The scientists identified nucleotide sequences from a pathogenic bacterium, Salmonella enterica serovar Typhi ((Figure)), which causes typhoid fever.1 This disease is commonly seen in overcrowded areas and has caused epidemics throughout recorded history.

Bubonic Plagues
From 541 to 750, the Plague of Justinian, an outbreak of what was likely bubonic plague, eliminated one-quarter to one-half of the human population in the eastern Mediterranean region. The population in Europe dropped by 50 percent during this outbreak. Astoundingly, bubonic plague would strike Europe more than once!
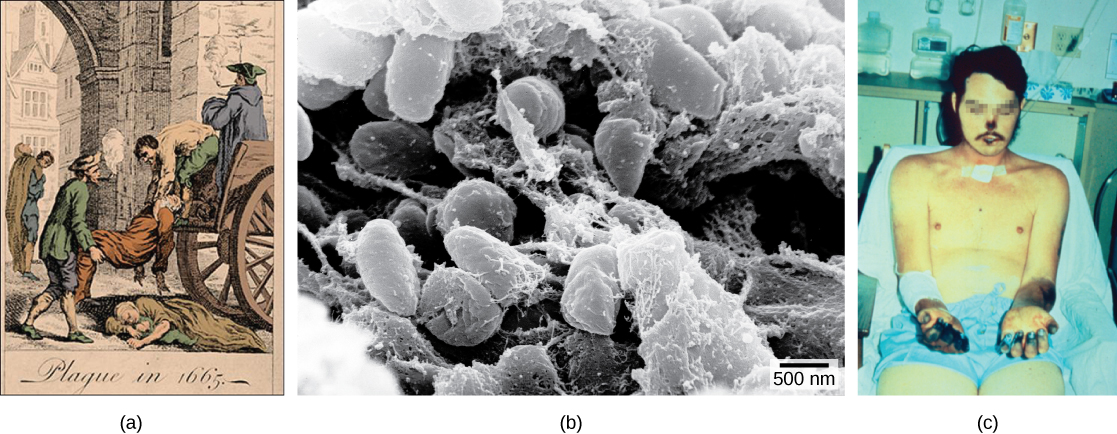
Bubonic plague is caused by the bacterium Yersinia pestis. One of the most devastating pandemics attributed to bubonic plague was the Black Death (1346 to 1361). It is thought to have originated in China and spread along the Silk Road, a network of land and sea trade routes, to the Mediterranean region and Europe, carried by fleas living on black rats that were always present on ships. The Black Death was probably named for the tissue necrosis ((Figure)c) that can be one of the symptoms. The “buboes” of bubonic plague were painfully swollen areas of lymphatic tissue. A pneumonic form of the plague, spread by the coughing and sneezing of infected individuals, spreads directly from human to human and can cause death within a week. The pneumonic form was responsible for the rapid spread of the Black Death in Europe. The Black Death reduced the world’s population from an estimated 450 million to about 350 to 375 million. Bubonic plague struck London yet again in the mid-1600s ((Figure)). In modern times, approximately 1,000 to 3,000 cases of plague arise globally each year, and a “sylvatic” form of plague, carried by fleas living on rodents such as prairie dogs and black footed ferrets, infects 10 to 20 people annually in the American Southwest. Although contracting bubonic plague before antibiotics meant almost certain death, the bacterium responds to several types of modern antibiotics, and mortality rates from plague are now very low.
Watch a video on the modern understanding of the Black Death—bubonic plague in Europe during the 14th century.
Migration of Diseases to New Populations
One of the negative consequences of human exploration was the accidental “biological warfare” that resulted from the transport of a pathogen into a population that had not previously been exposed to it. Over the centuries, Europeans tended to develop genetic immunity to endemic infectious diseases, but when European conquerors reached the western hemisphere, they brought with them disease-causing bacteria and viruses, which triggered epidemics that completely devastated many diverse populations of Native Americans, who had no natural resistance to many European diseases. It has been estimated that up to 90 percent of Native Americans died from infectious diseases after the arrival of Europeans, making conquest of the New World a foregone conclusion.
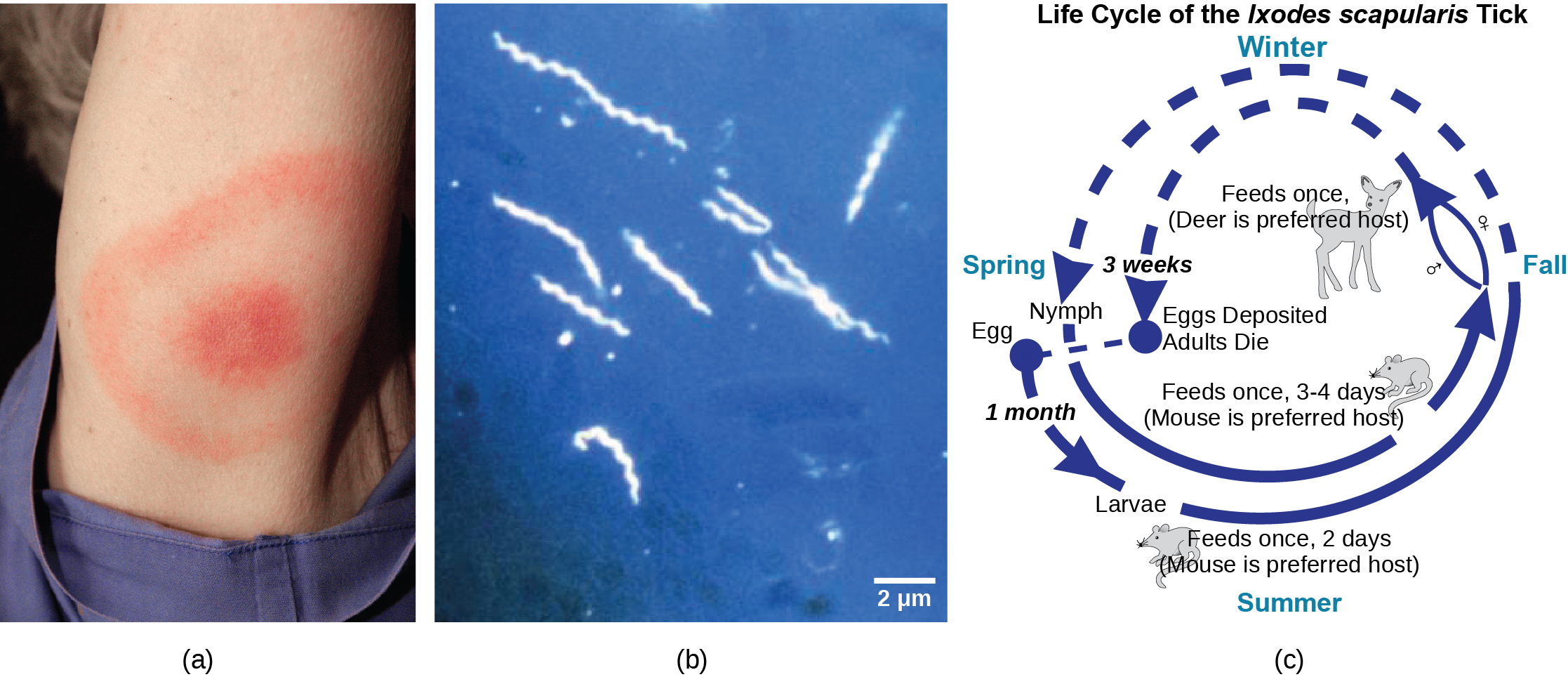
Emerging and Re-emerging Diseases
The distribution of a particular disease is dynamic. Changes in the environment, the pathogen, or the host population can dramatically impact the spread of a disease. According to the World Health Organization (WHO), an emerging disease ((Figure)) is one that has appeared in a population for the first time, or that may have existed previously but is rapidly increasing in incidence or geographic range. This definition also includes re-emerging diseases that were previously under control. Approximately 75 percent of recently emerging infectious diseases affecting humans are zoonotic diseases. Zoonoses are diseases that primarily infect animals but can be transmitted to humans; some are of viral origin and some are of bacterial origin. Brucellosis is an example of a prokaryotic zoonosis that is re-emerging in some regions, and necrotizing fasciitis (commonly known as flesh-eating bacteria) has been increasing in virulence for the last 80 years for unknown reasons.
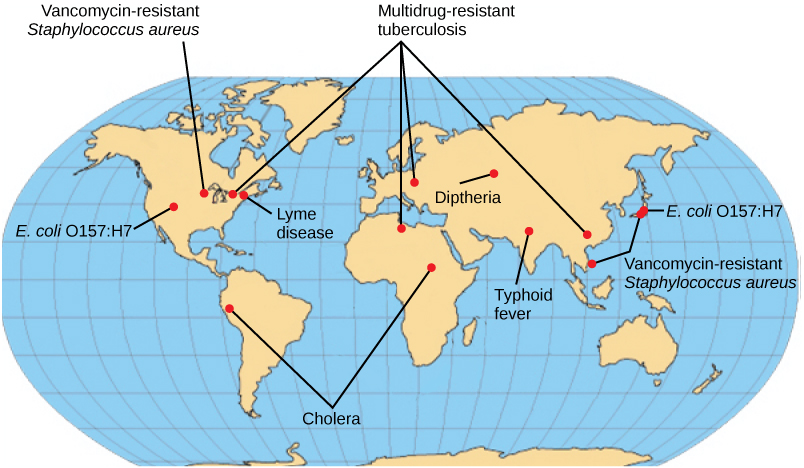
Some of the present emerging diseases are not actually new, but are diseases that were catastrophic in the past ((Figure)). They devastated populations and became dormant for a while, just to come back, sometimes more virulent than before, as was the case with bubonic plague. Other diseases, like tuberculosis, were never eradicated but were under control in some regions of the world until coming back, mostly in urban centers with high concentrations of immunocompromised people. WHO has identified certain diseases whose worldwide re-emergence should be monitored. Among these are three viral diseases (dengue fever, yellow fever, and zika), and three bacterial diseases (diphtheria, cholera, and bubonic plague). The war against infectious diseases has no foreseeable end.
Foodborne Diseases
Prokaryotes are everywhere: They readily colonize the surface of any type of material, and food is not an exception. Most of the time, prokaryotes colonize food and food-processing equipment in the form of a biofilm, as we have discussed earlier. Outbreaks of bacterial infection related to food consumption are common. A foodborne disease (commonly called “food poisoning”) is an illness resulting from the consumption the pathogenic bacteria, viruses, or other parasites that contaminate food. Although the United States has one of the safest food supplies in the world, the U.S. Centers for Disease Control and Prevention (CDC) has reported that “76 million people get sick, more than 300,000 are hospitalized, and 5,000 Americans die each year from foodborne illness.”
The characteristics of foodborne illnesses have changed over time. In the past, it was relatively common to hear about sporadic cases of botulism, the potentially fatal disease produced by a toxin from the anaerobic bacterium Clostridium botulinum. Some of the most common sources for this bacterium were non-acidic canned foods, homemade pickles, and processed meat and sausages. The can, jar, or package created a suitable anaerobic environment where Clostridium could grow. Proper sterilization and canning procedures have reduced the incidence of this disease.
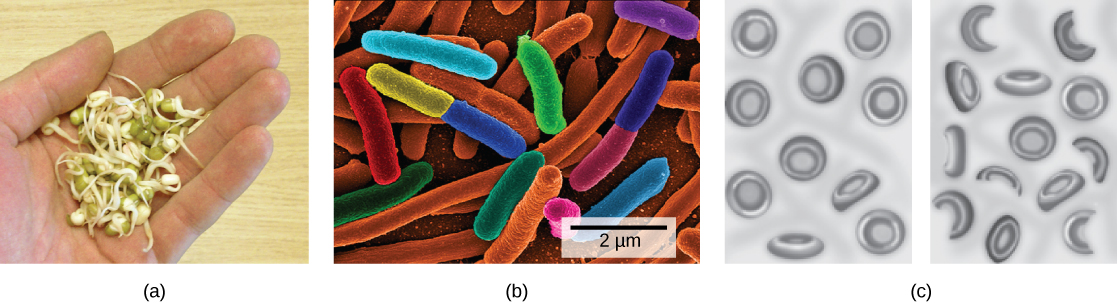
While people may tend to think of foodborne illnesses as associated with animal-based foods, most cases are now linked to produce. There have been serious, produce-related outbreaks associated with raw spinach in the United States and with vegetable sprouts in Germany, and these types of outbreaks have become more common. The raw spinach outbreak in 2006 was produced by the bacterium E. coli serotype O157:H7. A serotype is a strain of bacteria that carries a set of similar antigens on its cell surface, and there are often many different serotypes of a bacterial species. Most E. coli are not particularly dangerous to humans, but serotype O157:H7 can cause bloody diarrhea and is potentially fatal.
All types of food can potentially be contaminated with bacteria. Recent outbreaks of Salmonella reported by the CDC occurred in foods as diverse as peanut butter, alfalfa sprouts, and eggs. A deadly outbreak in Germany in 2010 was caused by E. coli contamination of vegetable sprouts ((Figure)). The strain that caused the outbreak was found to be a new serotype not previously involved in other outbreaks, which indicates that E. coli is continuously evolving. Outbreaks of listeriosis, due to contamination of meats, raw cheeses, and frozen or fresh vegetables with Listeria monocytogenes, are becoming more frequent.
Biofilms and Disease
Recall that biofilms are microbial communities that are very difficult to destroy. They are responsible for diseases such as Legionnaires’ disease, otitis media (ear infections), and various infections in patients with cystic fibrosis. They produce dental plaque and colonize catheters, prostheses, transcutaneous and orthopedic devices, contact lenses, and internal devices such as pacemakers. They also form in open wounds and burned tissue. In healthcare environments, biofilms grow on hemodialysis machines, mechanical ventilators, shunts, and other medical equipment. In fact, 65 percent of all infections acquired in the hospital (nosocomial infections) are attributed to biofilms. Biofilms are also related to diseases contracted from food because they colonize the surfaces of vegetable leaves and meat, as well as food-processing equipment that isn’t adequately cleaned.
Biofilm infections develop gradually and may not cause immediate symptoms. They are rarely resolved by host defense mechanisms. Once an infection by a biofilm is established, it is very difficult to eradicate, because biofilms tend to be resistant to most methods used to control microbial growth, including antibiotics. The matrix that attaches the cells to a substrate and to other another protects the cells from antibiotics or drugs. In addition, since biofilms grow slowly, they are less responsive to agents that interfere with cell growth. It has been reported that biofilms can resist up to 1,000 times the antibiotic concentrations used to kill the same bacteria when they are free-living or planktonic. An antibiotic dose that large would harm the patient; therefore, scientists are working on new ways to get rid of biofilms.
Antibiotics: Are We Facing a Crisis?
The word antibiotic comes from the Greek anti meaning “against” and bios meaning “life.” An antibiotic is a chemical, produced either by microbes or synthetically, that is hostile to or prevents the growth of other organisms. Today’s media often address concerns about an antibiotic crisis. Are the antibiotics that easily treated bacterial infections in the past becoming obsolete? Are there new “superbugs”—bacteria that have evolved to become more resistant to our arsenal of antibiotics? Is this the beginning of the end of antibiotics? All these questions challenge the healthcare community.
One of the main causes of antibiotic resistance in bacteria is overexposure to antibiotics. The imprudent and excessive use of antibiotics has resulted in the natural selection of resistant forms of bacteria. The antibiotic kills most of the infecting bacteria, and therefore only the resistant forms remain. These resistant forms reproduce, resulting in an increase in the proportion of resistant forms over non-resistant ones. In addition to transmission of resistance genes to progeny, lateral transfer of resistance genes on plasmids can rapidly spread these genes through a bacterial population. A major misuse of antibiotics is in patients with viral infections like colds or the flu, against which antibiotics are useless. Another problem is the excessive use of antibiotics in livestock. The routine use of antibiotics in animal feed promotes bacterial resistance as well. In the United States, 70 percent of the antibiotics produced are fed to animals. These antibiotics are given to livestock in low doses, which maximize the probability of resistance developing, and these resistant bacteria are readily transferred to humans.
Watch a recent news report on the problem of routine antibiotic administration to livestock and antibiotic-resistant bacteria.
One of the Superbugs: MRSA
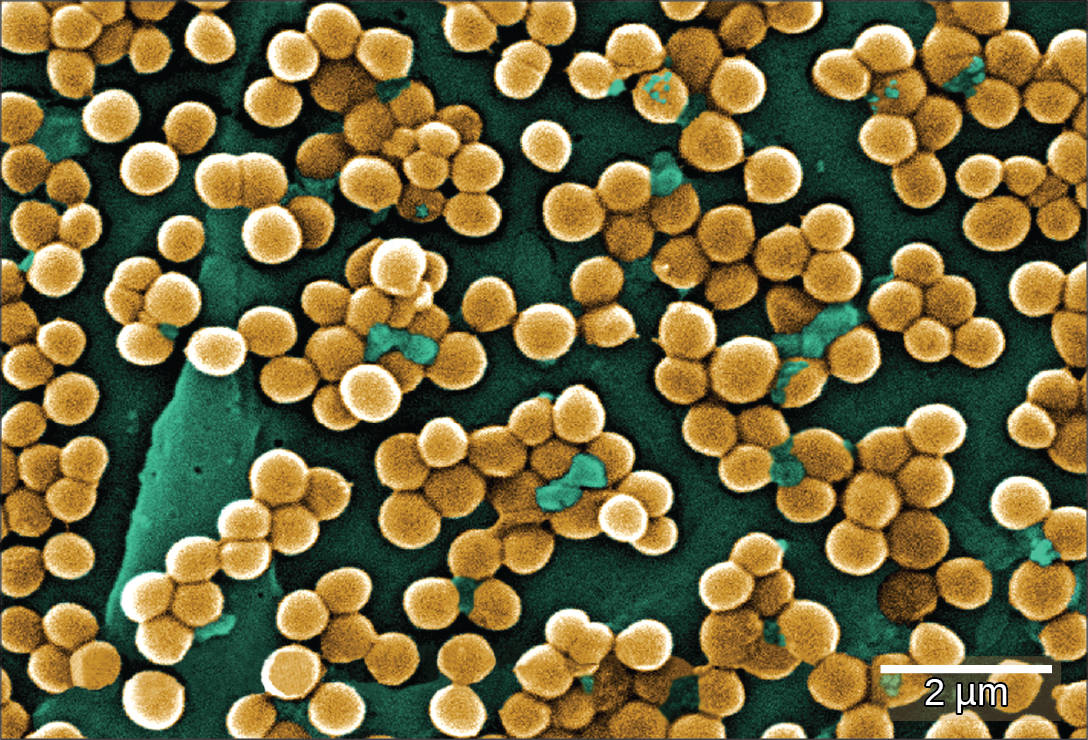
The imprudent use of antibiotics has paved the way for the expansion of resistant bacterial populations. For example, Staphylococcus aureus, often called “staph,” is a common bacterium that can live in the human body and is usually easily treated with antibiotics. However, a very dangerous strain, methicillin-resistant Staphylococcus aureus (MRSA) has made the news over the past few years ((Figure)). This strain is resistant to many commonly used antibiotics, including methicillin, amoxicillin, penicillin, and oxacillin. MRSA can cause infections of the skin, but it can also infect the bloodstream, lungs, urinary tract, or sites of injury. While MRSA infections are common among people in healthcare facilities, they have also appeared in healthy people who haven’t been hospitalized, but who live or work in tight populations (like military personnel and prisoners). Researchers have expressed concern about the way this latter source of MRSA targets a much younger population than those residing in care facilities. The Journal of the American Medical Association reported that, among MRSA-afflicted persons in healthcare facilities, the average age is 68, whereas people with “community-associated MRSA” (CA-MRSA) have an average age of 23.2
In summary, the medical community is facing an antibiotic crisis. Some scientists believe that after years of being protected from bacterial infections by antibiotics, we may be returning to a time in which a simple bacterial infection could again devastate the human population. Researchers are developing new antibiotics, but it takes many years of research and clinical trials, plus financial investments in the millions of dollars, to generate an effective and approved drug.
EpidemiologistEpidemiology is the study of the occurrence, distribution, and determinants of health and disease in a population. It is, therefore, part of public health. An epidemiologist studies the frequency and distribution of diseases within human populations and environments.
Epidemiologists collect data about a particular disease and track its spread to identify the original mode of transmission. They sometimes work in close collaboration with historians to try to understand the way a disease evolved geographically and over time, tracking the natural history of pathogens. They gather information from clinical records, patient interviews, surveillance, and any other available means. That information is used to develop strategies, such as vaccinations ((Figure)), and design public health policies to reduce the incidence of a disease or to prevent its spread. Epidemiologists also conduct rapid investigations in case of an outbreak to recommend immediate measures to control it.
An epidemiologist has a bachelor’s degree, plus a master’s degree in public health (MPH). Many epidemiologists are also physicians (and have an M.D. or D.O degree), or they have a Ph.D. in an associated field, such as biology or microbiology.

Section Summary
Some prokaryotes are human pathogens. Devastating diseases and plagues have been among us since early times and remain among the leading causes of death worldwide. Emerging diseases are those rapidly increasing in incidence or geographic range. They can be new or re-emerging diseases (previously under control). Many emerging diseases affecting humans originate in animals (zoonoses), such as brucellosis. A group of re-emerging bacterial diseases recently identified by WHO for monitoring include bubonic plague, diphtheria, and cholera. Foodborne diseases result from the consumption of food contaminated with food, pathogenic bacteria, viruses, or parasites.
Some bacterial infections have been associated with biofilms: Legionnaires’ disease, otitis media, and infection of patients with cystic fibrosis. Biofilms can grow on human tissues, like dental plaque; colonize medical devices; and cause infection or produce foodborne disease by growing on the surfaces of food and food-processing equipment. Biofilms are resistant to most of the methods used to control microbial growth. The excessive use of antibiotics has resulted in a major global problem, since resistant forms of bacteria have been selected over time. A very dangerous strain, methicillin-resistant Staphylococcus aureus (MRSA), has wreaked havoc recently across the world.
Review Questions
A disease that is constantly present in a population is called _____.
- pandemic
- epidemic
- endemic
- re-emerging
C
Which of the statements about biofilms is incorrect?
- Biofilms are considered responsible for diseases such as cystic fibrosis.
- Biofilms produce dental plaque, and colonize catheters and prostheses.
- Biofilms colonize open wounds and burned tissue.
- All statements are incorrect.
D
Which of these statements is true?
- An antibiotic is any substance produced by a organism that is antagonistic to the growth of prokaryotes.
- An antibiotic is any substance produced by a prokaryote that is antagonistic to the growth of other viruses.
- An antibiotic is any substance produced by a prokaryote that is antagonistic to the growth of eukaryotic cells.
- An antibiotic is any substance produced by a prokaryote that prevents growth of the same prokaryote.
A
A person in England arrives at a medical clinic with a fever and swollen lymph nodes shortly after returning from a visit to New Mexico. For which bacteria should the doctor test the patient?
- Salmonella enterica
- Borrelia burgdorferi
- Clostridium botulinum
- Yersinia pestis
D
MRSA has emerged as a serious infectious disease, with the first case of methicillin-resistant S. aureus being detected in 1961. Why are medical professionals so concerned when antibiotics exist that can kill MRSA?
- MRSA can transfer methicillin-resistance to other bacteria.
- Patients are not treated with correct antibiotics rapidly enough to prevent serious illness.
- MRSA could acquire additional antibiotic resistance genes from other bacteria to become a “super bug.”
- All of the above.
D
Critical Thinking Questions
Explain the reason why the imprudent and excessive use of antibiotics has resulted in a major global problem.
Antibiotics kill bacteria that are sensitive to them; thus, only the resistant ones will survive. These resistant bacteria will reproduce, and therefore, after a while, there will be only resistant bacteria.
Researchers have discovered that washing spinach with water several times does not prevent foodborne diseases due to E. coli. How can you explain this fact?
E. coli colonizes the surface of the leaf, forming a biofilm that is more difficult to remove than free (planktonic) cells. Additionally, bacteria can be taken up in the water that plants are grown in, thereby entering the plant tissues rather than simply residing on the leaf surface.
Footnotes
- 1 Papagrigorakis MJ, Synodinos PN, and Yapijakis C. Ancient typhoid epidemic reveals possible ancestral strain of Salmonella enterica serovar Typhi. Infect Genet Evol 7 (2007): 126–7, Epub 2006 Jun.
- 2 Naimi, TS, LeDell, KH, Como-Sabetti, K, et al. Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA 290 (2003): 2976–84, doi: 10.1001/jama.290.22.2976.
Glossary
- antibiotic
- biological substance that, in low concentration, is antagonistic to the growth of prokaryotes
- Black Death
- devastating pandemic that is believed to have been an outbreak of bubonic plague caused by the bacterium Yersinia pestis
- botulism
- disease produced by the toxin of the anaerobic bacterium Clostridium botulinum
- CA-MRSA
- MRSA acquired in the community rather than in a hospital
- emerging disease
- disease making an initial appearance in a population or that is increasing in incidence or geographic range
- endemic disease
- disease that is constantly present, usually at low incidence, in a population
- epidemic
- disease that occurs in an unusually high number of individuals in a population at the same time
- foodborne disease
- any illness resulting from the consumption of contaminated food, or of the pathogenic bacteria, viruses, or other parasites that contaminate food
- MRSA
- (methicillin-resistant Staphylococcus aureus) very dangerous Staphylococcus aureus strain resistant to multiple antibiotics
- pandemic
- widespread, usually worldwide, epidemic disease
- serotype
- strain of bacterium that carries a set of similar antigens on its cell surface, often many in a bacterial species
- zoonosis
- disease that primarily infects animals that is transmitted to humans

